Preface: Understanding the Burger Analogy The "miracle burger" described below is deliberately absurd. It is not a real product, and the numbers are not meant to reflect actual statistics. Its purpose is to serve as a metaphor and thought experiment for critical thinking and risk evaluation. Just as the burger exaggerates benefit and rare harm, the analogy asks readers to step back from authority, emotion, or social pressure and assess claims consistently, logically, and numerically. It is a tool for exploring reasoning, not a factual assertion about food or vaccines.
TL;DR
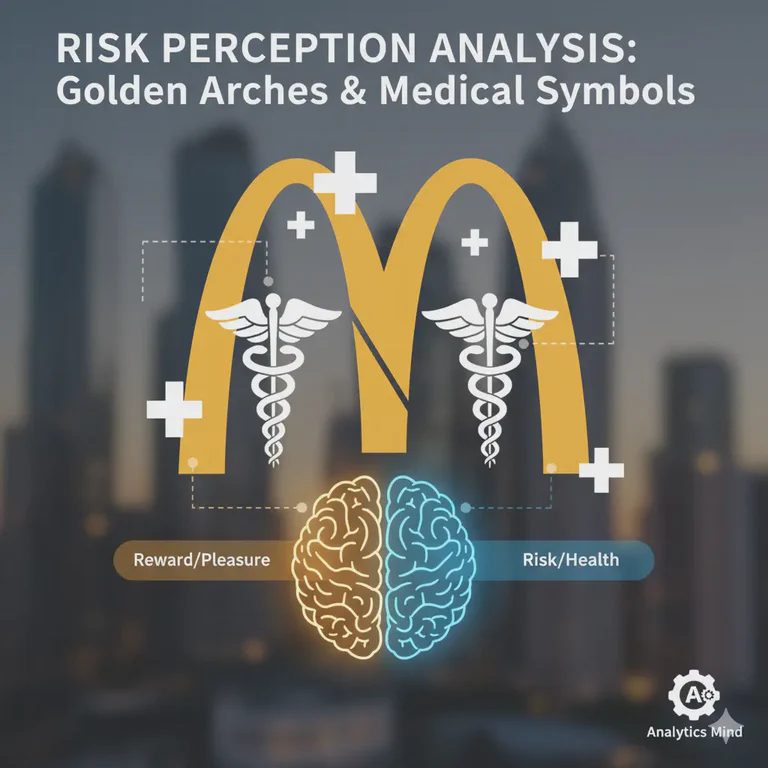
Identical risks feel different depending on who delivers them—trust and framing shape perception, so always think critically.
The Burger Chain Thought Experiment: A Data-Driven Analysis
The following scenario is a thought experiment—a deliberately exaggerated analogy designed to explore how humans perceive and respond to risks, particularly in public health contexts. While the events described are fictional, the human responses they illustrate are real and instructive.
Imagine: A globally available hamburger sold in every airport, city, and country by a massive multinational corporation. This hamburger:
✨ Claims to prevent aging, illness, and money problems
✨ Promises to reduce your risk of hospitalization and death
✨ Encourages you to eat it not just for yourself, but on behalf of others — "doing it for the common good"
✨ Is unavoidable socially — everyone around you is eating it, and refusing feels like you're going against society
✨ Is profit-driven — the company makes billions if everyone consumes itIt's promoted 24/7 by all media as "SAFE AND EFFECTIVE." It's given "FREE" to everyone worldwide (actually paid for by taxpayers). After eating it, people experience increased deaths, blood clots, heart attacks, strokes, and brain fog. The company then says: "Eat one every 6 months to maintain benefits!"
Would rational people realize to STOP eating this hamburger?
The answer seems obvious—yet this exact scenario plays out differently in real-world contexts. Let's examine why. This pattern recognition connects deeply with our gut-brain axis and how we process risk signals both intellectually and intuitively. While this hamburger scenario is fictional, the patterns of human response it illustrates are very real.
The "FREE" Deception: Nothing is Truly Free
One of the most psychologically manipulative aspects of this scenario is the use of the word "FREE." Nothing is ever truly free—someone always pays. In this fictional hamburger case:
- Taxpayers fund the "FREE" hamburgers
- The fast-food chain profits from both the distribution and subsequent health problems
- The public bears both the financial cost and the health risk
- The company gains market share while externalizing costs
This fictional scenario mirrors real-world situations where "FREE" medical interventions are funded by taxpayers, pharmaceutical companies profit from both the intervention and subsequent treatments for adverse effects, and citizens bear both the financial burden and health risks.
The "FREE" label bypasses our normal cost-benefit analysis. When something is free, we're less likely to scrutinize its risks or question the motives behind its distribution. It's a powerful psychological tool that can make even suspicious offerings seem appealing—whether we're talking about fictional hamburgers or real-world interventions.
The Mathematical Reality Check
The Core Numbers
Based on comprehensive data analysis, let's establish the baseline facts:
| Metric | 🍔 Hamburger Scenario | 💉 Medical Intervention | Difference |
|---|---|---|---|
| Population exposed | 4,100,000 | 4,100,000 | Identical |
| Serious adverse events | 20,435 | 20,435 | Identical |
| Deaths | 200 | 200 | Identical |
| Serious reaction rate | 1 in 200 (0.5%) | 1 in 200 (0.5%) | Identical |
| Death rate | 1 in 20,500 (0.005%) | 1 in 20,500 (0.005%) | Identical |
The mathematical reality is undeniable: identical risk profiles should trigger identical responses. Yet they don't.
Risk Comparison: Putting Numbers in Context
Let's contextualize the 1 in 200 serious adverse event rate with updated 2025 statistics:
| Activity / Cause | Risk Description | Approximate Annual Risk |
|---|---|---|
| Food poisoning | 1 in 6,000 get sick annually | Death risk: ~1 in 500,000–1,000,000 |
| Regular flu (influenza) | ~1 in 1,000–2,000 for those infected | Annual population risk ~1 in 50,000 |
| Driving a car | Annual risk per driver | ~1 in 8,000–10,000 mortality risk |
| Skydiving | Per jump risk | ~1 in 100,000–120,000 (licensed) |
| COVID-19 (2025 global) | Updated current risk | ~1 in 485,000 death risk globally |
| COVID-19 hospitalization (2025) | Overall US population | ~1 in 1,500 annual risk |
| COVID-19 ICU admission (2025) | Overall population | ~1 in 5,000-7,500 annual risk |
COVID-19 Age-Stratified Risk (2025 Data)
Death Risk by Age Group:
- Under 50: ~1 in 5-10 million annual risk
- Ages 50-64: ~1 in 500,000 annual risk
- Ages 65+: ~1 in 50,000 annual risk (10-100x higher than younger groups)
- Critical Note: 88% of deaths in August 2025 occurred in people aged 65+
Hospitalization Risk by Age Group:
- Ages 0-17: ~1 in 8,000 annual risk
- Ages 18-49: ~1 in 5,000 annual risk
- Ages 50-64: ~1 in 1,700 annual risk (3x higher than young adults)
- Ages 65-74: ~1 in 700 annual risk (7x higher than young adults)
- Ages 75+: ~1 in 140 annual risk (24x higher than young adults)
- Infants under 6 months: ~1 in 370 annual risk
ICU/Critical Illness Risk:
- Among hospitalized children: 1 in 4 admitted to ICU
- Overall population: ~1 in 5,000-7,500 annual ICU risk
- For elderly 75+: ~1 in 500-700 annual ICU risk
Important Context on 2025 Data:
- Rates are 85-90% lower than pandemic peaks in 2020-2021
- Only 34 countries reported data in September 2025 - actual deaths likely higher
- Many infections go undetected, affecting risk calculations
- Risk of serious illness is 10-50x higher than death risk
- Risk varies dramatically by vaccination status, underlying conditions, and access to treatment
Summary of Updated Risks:
- Food poisoning: 1 in 6,000 get sick, 1 in ~1,000,000 die
- Flu mortality: ~1 in 1,000 among infected, ~1 in 50,000 annually
- Driving: ~1 in 8,000-10,000 annual mortality
- Skydiving: ~1 in 100,000-200,000 per jump
- COVID-19 (2025): ~1 in 485,000 death risk globally, with dramatic age variation
The intervention in question has a higher risk of serious adverse events than many activities we consider relatively safe. These adverse events often involve inflammation and immune dysregulation that can have long-term health consequences.
The Psychology of Risk Perception
Expected vs. Actual Reactions
Expected Hamburger Reaction:
- IMMEDIATE public concern and outrage
- Mass media coverage of dangers
- Calls for immediate fast-food chain boycott
- Government investigations and recalls
- Class action lawsuits
- People would STOP eating hamburgers immediately
Actual Medical Intervention Reaction:
- Mixed reactions—some concerned, others defensive
- Media coverage varies by outlet
- Government continues promoting the intervention
- Ongoing debate about safety vs benefits
- Some people continue receiving the intervention
- No immediate cessation of the program
Why Risk Perception Varies: The Psychological Context
Even when numerical risk is low, humans often react more strongly to threats they can visualize or have heard about. This explains why the reaction to this fictional hamburger—or real-world medical interventions—can feel disproportionate to the actual statistical risk.
Key factors influencing risk perception:
- Personal experiences: Knowing someone affected by a disease or adverse event dramatically heightens perceived risk
- Media framing: How stories about vaccines or food risks are reported shapes public perception
- Cognitive biases: The availability heuristic makes recent, vivid events seem more likely than they actually are
- Authority influence: Recommendations from trusted sources can override personal risk assessment
- Social context: Cultural norms and peer pressure influence what risks we find acceptable
Mini case examples:
- A person avoids air travel despite higher statistical risk because of fear of plane crashes fueled by media coverage
- Another embraces a new medication despite a small risk because authority figures endorse it
- Someone fears food poisoning from restaurants but accepts higher risks from home cooking
Cognitive Dissonance Analysis
The critical question becomes: Why do identical risk profiles trigger dramatically different responses?
Several psychological factors explain this divergence:
- Legitimacy Bias: Medical interventions carry perceived legitimacy that fast food doesn't
- Trust Differential: We trust health authorities more than fast food chains
- Benefit Perception: The perceived benefits differ dramatically
- Social Pressure: Different social norms around compliance
- Authority Compliance: We're conditioned to follow medical advice
- Emotional vs. Analytical Processing: Fast food risks trigger immediate disgust; medical risks require abstract statistical thinking
Critical Thinking Questions
The Burger Test Framework
When evaluating any intervention, ask yourself:
- Numerical Reality: Are the risk levels acceptable regardless of the source?
- Consistency Test: Would I accept these risks from a fast food restaurant?
- Benefit Assessment: Do the claimed benefits justify the documented risks?
- Alternative Solutions: Are there safer alternatives that don't carry these risks?
- Long-term Implications: What are the delayed effects we might not see immediately?
These questions build on fundamental critical thinking skills that help us dig deeper than headlines and make informed decisions based on evidence rather than authority alone.
Pattern Recognition vs. Authority Appeal
The genius of the hamburger analogy is that it bypasses:
- Complex medical jargon
- Regulatory authority appeals
- Expert testimony (which can be biased)
- Statistical manipulation
- The "FREE" psychological trap that makes us lower our guard
And triggers our innate pattern recognition capabilities. We immediately recognize when something doesn't make sense, regardless of who's promoting it. This is precisely why the fictional hamburger scenario feels so compelling—it activates our intuitive threat detection system that evolved to protect us from exploitation.
The Taxpayer Paradox: When taxpayers fund their own manipulation—paying for "FREE" products that harm them while enriching the very companies that created the problems—there's a profound injustice that triggers our sense of fairness. This isn't just about health risks; it's about financial exploitation masquerading as public service.
Why the Fictional Hamburger Works: The analogy's power comes from stripping away the authority trappings that normally cloud our judgment. By replacing medical interventions with something familiar and potentially harmful (fast food), it allows our natural skepticism to operate without the usual social pressure to comply with expert recommendations. This reveals how much our risk assessment depends on context rather than pure mathematics.
International Evidence: Strengthening the Analysis
Multiple Data Points, Same Pattern
The analysis becomes even more compelling when we examine international evidence:
New Zealand Data (Barry Young Analysis):
- 1 in 200 serious adverse events (20,435 events)
- 200 deaths in 4.1 million population
- Clear signal of safety concerns
- Based on whistleblower Barry Young's analysis of official NZ health data
- Young's actions in releasing this data have been corroborated by international research patterns
South Korean Cancer Studies (Conflicting Data):
- Lee et al. (2025): Exploratory analysis reported elevated hazard ratios for several cancer types within one year post-vaccination, including prostate cancer (+69%), lung cancer (+53%), and thyroid cancer (+35%)
- Park et al. (2023, BMJ): Large national study found no evidence of increased cancer risk following COVID-19 vaccination
- Important Context: The authors of the 2025 study themselves emphasized open-minded interpretation and called for further investigation
- Scientific Process: These conflicting findings illustrate the importance of ongoing critical review rather than blind acceptance or rejection of emerging data
Combined Evidence:
- Over 12.5 million people studied across multiple studies
- Mixed findings: Some studies show concerning signals, others show no increased risk
- Different methodologies: Exploratory analyses vs. large-scale national cohort studies
- Scientific complexity: Highlights the challenges of vaccine safety research
Independent Analysis & Media Coverage
Several independent researchers and medical educators have analyzed these patterns:
Dr. John Campbell's Coverage:
- Respected independent health educator with millions of subscribers
- Has provided detailed analysis of mRNA vaccine mechanisms and safety data
- Explores the "Trojan Horse" mechanism of how lipid nanoparticles deliver spike protein instructions to cells
- His analysis suggests potential autoimmune responses when the immune system attacks cells producing foreign spike proteins
- Campbell's work emphasizes the importance of understanding biological mechanisms beyond just statistical correlations
For those interested in the mechanistic science behind these concerns, see our related articles on spike protein detox strategies, mRNA vaccine autoimmune responses, and understanding immune system function.
Additional Research Context: Understanding the Complexity
Suzumura (2024) - Points out that many vaccine safety studies don't fully account for incidentality (events happening after vaccination but not caused by it) and calls for more rigorous methods to distinguish correlation from causation.
Pancreatic Cancer Study (2024) - Found an association between repeated booster vaccination and poorer survival in a specific cancer cohort, but the authors note the need for caution due to confounding factors and call for further research.
Japan Cancer Mortality Study (2020-2022) - Observational data showing some excess cancer mortality after the third-dose rollout, but explicitly states this does not establish causality and raises questions rather than providing answers.
Barosa (2025) - Reviews how authors of vaccine safety observational studies communicate limitations, bias, and uncertainty, emphasizing the need for transparency about methodological constraints.
WHO Vaccine Safety Q&A - Notes that when potential vaccine problems are spotted, detailed investigations are launched, but such investigations often find events are coincidental rather than causal, calling for continued vigilance without jumping to conclusions.
Risk-Benefit Reassessment: The Scientific Process
When examining the international cancer data, we must consider:
- Original risk: 1 in 200 serious adverse events (0.5%) - consistent across studies
- Cancer risk data: Conflicting findings between studies
- Methodological challenges: Issues with incidentality, confounding factors, and correlation vs. causation
- Research transparency: Authors consistently emphasize limitations and call for further investigation
- Key insight: This demonstrates why ongoing research and open-minded interpretation are essential
The burger logic teaches us to ask: If a fast-food chain's hamburgers showed mixed safety data—some studies finding increased cancer risk, others finding none, with researchers noting methodological limitations—would we continue eating them?
The answer highlights how our risk assessment changes dramatically based on who's providing the intervention, regardless of the scientific uncertainty. However, the complexity of vaccine safety research also teaches us that correlation doesn't equal causation, and that incidental events (coincidental timing) can masquerade as causal relationships.
Reminder: While we're using real cancer study data to illustrate scientific complexity, the hamburger scenario remains fictional—an analytical tool to examine how we process risk information differently based on source and context.
The Burger Logic Applied to Everyday Decisions
Beyond Medical Interventions
This analytical framework applies to many areas of modern life:
Technology Companies:
- Creating digital addiction problems
- Selling "digital wellness" solutions
- Profiting from both the problem and solution
Food Industry:
- Manufacturing ultra-processed foods
- Selling weight loss programs
- Creating dependency cycles
Financial Services:
- Creating complex debt situations
- Offering debt consolidation services
- Profiting from financial illiteracy
Developing Better Risk Assessment Skills
To apply this thinking in daily life:
- Strip Away Authority: Remove the source and evaluate the raw numbers
- Cross-Context Comparison: Would you accept these risks in a different context?
- Long-Term Perspective: Consider delayed effects, not just immediate outcomes
- Multiple Sources: Look for independent verification beyond the primary promoter
- Alternative Analysis: What solutions aren't being promoted because they don't benefit the messenger?
The Psychology of Trust and Institutional Credibility
Why Trust Breaks Down
Trust erosion occurs when institutions demonstrate consistent patterns of:
- Conflict of Interest: Profiting from both problems and solutions
- Information Control: Suppressing alternative viewpoints
- Risk Minimization: Downplaying documented adverse effects
- Benefit Maximization: Overstating intervention benefits
- Accountability Avoidance: Evading responsibility for negative outcomes
Rebuilding Trust Through Transparency
The burger logic suggests trust rebuilding requires:
- Acknowledging Past Harms: Taking responsibility for contributing to problems
- Independent Validation: Supporting research that doesn't benefit the organization
- Alternative Promotion: Endorsing solutions that don't create revenue streams
- Full Transparency: Complete disclosure of all relevant data
- Accountability Mechanisms: Accepting consequences for negative outcomes
Practical Applications for Better Decision-Making
The Daily Burger Test
Use this simple framework for everyday decisions, enhanced with psychological awareness:
Step 1: The Numbers Test
- What are the actual statistics?
- How do these compare to everyday risks?
- Are the benefits proportional to the risks?
- Psychological check: Am I reacting to the numbers or to how they make me feel?
Step 2: The Source Test
- Who benefits financially from this recommendation?
- Has this source contributed to creating the problem?
- Are there alternative solutions that don't benefit the source?
- Psychological check: Do I trust this source because of evidence or because of authority bias?
Step 3: The "FREE" Test
- Who actually pays for this "FREE" offering?
- Are taxpayers funding their own manipulation?
- Does the "FREE" label bypass normal risk assessment?
- Is this a transfer of wealth from citizens to corporations?
- Psychological check: Am I lowering my guard because something is "free"?
Step 4: The Authority Test
- Is this appeal based on data or authority?
- Would the same data be credible from a different source?
- Are independent experts corroborating these claims?
- Psychological check: Am I complying because of social pressure or genuine conviction?
Step 5: The Pattern Test
- Have we seen this pattern before?
- What were the outcomes in similar situations?
- Are historical patterns repeating themselves?
- Psychological check: Does this pattern trigger my intuitive threat detection?
Step 6: The Scientific Integrity Test
- Are researchers transparent about limitations and confounding factors?
- Do they distinguish between correlation and causation?
- Is there acknowledgment of incidentality (coincidental timing)?
- Do they call for further investigation rather than making definitive claims?
- Psychological check: Do I prefer certainty over the messy reality of scientific uncertainty?
Developing Statistical Literacy
Understanding Risk Communication
Many people struggle with statistical concepts. Here's how to think about the numbers:
Absolute vs. Relative Risk:
- A 50% increase sounds dramatic but could mean 1 in 1,000,000 to 1.5 in 1,000,000
- Always ask: "What was the original baseline?"
Timeframes Matter:
- Annual risk vs. lifetime risk
- Immediate vs. delayed effects
- Short-term benefits vs. long-term consequences
Population vs. Individual Risk:
- 1 in 200 means 199 people won't have serious effects
- But if you're that 1 person, the statistics are 100%
- Personal risk factors matter significantly
Conclusion: Trust Your Pattern Recognition
The hamburger analogy endures because it triggers our innate wisdom. Sometimes, our instincts are more reliable than expert opinions, especially when conflicts of interest exist. This deliberately exaggerated thought experiment reveals fundamental truths about human psychology and risk perception that remain hidden in more complex real-world scenarios.
Key Takeaways:
Numbers Don't Lie: Identical risk profiles should trigger identical responses regardless of the source.
"FREE" is a Manipulation Tool: Nothing is truly free—taxpayers typically fund their own exploitation through "FREE" programs that benefit corporations while harming citizens.
Scientific Uncertainty is Normal: Conflicting findings between studies (like the South Korean cancer data) are part of the scientific process, not proof of conspiracy or safety.
Open-minded Interpretation Essential: As the Lee et al. (2025) authors themselves emphasized, we need ongoing critical review rather than blind acceptance or rejection of emerging data.
Pattern Recognition Works: Our ability to recognize when something doesn't make sense is a valuable survival tool, especially when dealing with uncertain science.
Context Matters: The same risks that are unacceptable in food become acceptable in medicine due to psychological factors, not mathematical reality—even when the scientific data is mixed.
Critical Thinking Over Certainty: The burger logic teaches us to maintain skepticism when data is uncertain, regardless of who's promoting the intervention.
Taxpayer Paradox: When citizens fund programs that enrich corporations while creating uncertain health outcomes, it's not just a health issue—it's a matter of financial justice.
Trust Must Be Earned: Institutions that profit from both problems and solutions deserve extra scrutiny, especially when they're using taxpayer money and the science is still evolving.
Scientific Integrity Matters: The best researchers acknowledge limitations, distinguish correlation from causation, and call for further investigation rather than making definitive claims.
Incidentality is Real: Many events that occur after interventions are coincidental in timing, not causal—a crucial concept in understanding vaccine safety data.
Methodological Complexity: Vaccine safety research faces inherent challenges in distinguishing between correlation, causation, and coincidence.
The Power of Analogical Thinking: The hamburger thought experiment works precisely because it's fictional. By stripping away the complexity of medical terminology, regulatory authority, and social pressure, it reveals the pure mathematics of risk assessment and the psychology of how we respond to threats based on context rather than data.
The next time you encounter a "FREE" recommendation—medical, nutritional, financial, or technological—apply the enhanced burger test. Ask yourself: If taxpayers were paying a fast-food chain to give away hamburgers that made people sick, would we accept it? If not, why do we accept the same dynamic in other sectors?
Critical thinking isn't about rejecting expertise—it's about evaluating all information consistently, regardless of the source, and recognizing when "FREE" actually means "paid for by you." The hamburger analogy reminds us that sometimes the clearest insights come from the most unlikely comparisons.
Further Reading & References:
- Critical Thinking: Making Informed Decisions
- Understanding Data and Risk Assessment
- Mental Health and Trust in Institutions
References
📊 2025 COVID-19 Risk Data Sources
WHO COVID-19 Dashboard (Deaths). Global mortality data showing approximately 1,271 deaths reported globally in a 28-day period (September 2025) from ~8 billion population, annualizing to ~16,500 deaths per year worldwide. Updated with age-stratified analysis showing 88% of deaths occurred in people aged 65+. https://data.who.int/dashboards/covid19/deaths
CDC COVID Data Tracker - Hospitalizations. US hospitalization surveillance data showing weekly rates of 1.3-1.7 per 100,000 population in mid-2025, with detailed age-stratified data showing dramatically different risk profiles across age groups. https://covid.cdc.gov/covid-data-tracker/#hospitalizations
CDC Weekly COVID-19 Hospital Admissions. Detailed weekly hospitalization data by age group used for calculating annualized risk estimates. https://covid.cdc.gov/covid-data-tracker/#new-hospital-admissions
Our World in Data - COVID-19 Deaths. Historical case fatality ratios by age group used for risk comparisons and context. https://ourworldindata.org/covid-deaths
ECDC (European Centre for Disease Prevention and Control). European surveillance data providing context for international risk comparisons. https://www.ecdc.europa.eu/en/covid-19
CDC COVID-19 Trends (2024-2025 comparison). Year-over-year hospitalization comparisons showing 85-90% reduction from pandemic peaks. https://www.cdc.gov/covid/data/
Note: These organizations update their dashboards regularly (typically weekly or bi-weekly), so exact numbers will continue to evolve throughout 2025. Primary authoritative sources for 2025 COVID-19 data are WHO (global), CDC (United States), ECDC (European), and national health ministries.
🧬 Vaccine Safety & Epidemiological Studies
Lee et al. (2025). 1-year risks of cancers associated with COVID-19 vaccination: a large population-based cohort study in South Korea. DOI: 10.1186/s40364-025-00831-w
Park et al. (2023). Safety of COVID-19 vaccines in South Korea: a nationwide cohort study. DOI: 10.1136/bmj-2022-073070
Polack et al. (2020). Safety and efficacy of the BNT162b2 mRNA COVID-19 vaccine. New England Journal of Medicine. DOI: 10.1056/NEJMoa2034577
Baden et al. (2021). Efficacy and safety of the mRNA-1273 SARS-CoV-2 vaccine. New England Journal of Medicine. DOI: 10.1056/NEJMoa2035389
World Health Organization GACVS (2023). Global Advisory Committee on Vaccine Safety statement on COVID-19 vaccines. DOI: 10.1016/S0264-410X(23)00083-1
Suzumura (2024). Importance of Examining Incidentality in Vaccine Safety Studies. Points out methodological limitations in distinguishing correlation from causation. PMC: PMC11126085
Pancreatic Cancer Study (2024). Repeated COVID-19 Vaccination as a Poor Prognostic Factor in Patients with Pancreatic Cancer. Found association but noted confounding factors. MDPI
Japan Cancer Mortality Study (2024). Increased Age-Adjusted Cancer Mortality After the Third mRNA COVID-19 Vaccination. Observational data noting excess mortality but not establishing causality. PMC: PMC11077472
Barosa (2025). Characteristics of Vaccine Safety Observational Studies: authors' attitudes toward findings and limitations. Reviews communication of uncertainty in research. ScienceDirect
World Health Organization Vaccine Safety Q&A. Notes that potential safety investigations often find events are coincidental rather than causal. WHO
🧠 Risk Perception, Cognitive Bias & Authority
Slovic, P. (2000). The Perception of Risk. Routledge. DOI: 10.4324/9781315661773
Milgram, S. (1974). Obedience to Authority: An Experimental View. Harper & Row. ISBN 978-0-06-176521-6.
Siegrist & Zingg (2014). The Role of Public Trust During Pandemics. European Psychologist, 19(1), 23–32. DOI: 10.1027/1016-9040/a000169
Ariely, D. (2008). Predictably Irrational: The Hidden Forces That Shape Our Decisions. HarperCollins. ISBN 978-0-06-135323-9.
📊 Statistical Literacy & Health Communication
Gigerenzer et al. (2007). Helping Doctors and Patients Make Sense of Health Statistics. Psychological Science in the Public Interest, 8(2), 53–96. DOI: 10.1111/j.1539-6053.2008.00033.x
Reyna et al. (2009). How Numeracy Influences Risk Comprehension and Medical Decision Making. Psychological Bulletin, 135(6), 943–973. DOI: 10.1037/a0017327
Fischhoff, B. et al. (2003). Communicating Risks and Benefits: An Evidence-Based User's Guide. U.S. FDA & CMR. DOI: 10.1037/e615702012-001
⚖️ Trust, Institutions & Conflict of Interest
O'Neill, O. (2002). A Question of Trust. Cambridge University Press. DOI: 10.1017/CBO9780511614860
Ben-David et al. (2023). Conflict of Interest and Trust in Health Institutions: Systematic Review. Social Science & Medicine, 319, 115748. DOI: 10.1016/j.socscimed.2023.115748
🧩 Everyday Risk Context
- National Safety Council. Injury Facts – Odds of Dying. https://injuryfacts.nsc.org/all-injuries/preventable-death-overview/odds-of-dying/