Timeline of Key Discoveries
- Ancient Times: Early observations of the spleen as a mysterious organ, often linked to blood and immunity. Hippocrates, the "father of medicine," noted the spleen's association with various diseases, though its precise function remained enigmatic.
- 17th Century: Initial anatomical studies of the spleen by pioneers in the field. Marcello Malpighi, an Italian physician, provided detailed anatomical descriptions of the spleen's structure, using the newly invented microscope, laying the groundwork for understanding its complex architecture.
- 19th Century: Discovery of the spleen's role in filtering blood and removing old cells, laying the groundwork for its function in immune surveillance. Gabriel Andral, a French pathologist, identified the spleen's role in clearing aged red blood cells, recognizing it as an important component of the reticuloendothelial system (now known as the mononuclear phagocyte system). 🩸
- Early 20th Century: Recognition of the spleen's involvement in immune responses, particularly antibody production. Paul Ehrlich, a German physician and immunologist (Nobel laureate), identified the spleen as a key site for antibody production, demonstrating the organ’s active role in humoral immunity (antibody-mediated immunity). ️
- 1950-1970s: A period of growing understanding of the gut's role in immune development. The work of scientists such as Robert Good and Jacques Miller further highlighted the importance of the gut-associated lymphoid tissue (GALT) in the development of the immune system.
- Mid-20th Century: The emergence of research linking the gut microbiome to immune development and function. Researchers like René Dubos, a pioneer in microbial ecology, began exploring the complex interactions between the gut microbiome and the host's immune system, highlighting the concept of "ecological balance".
- Late 20th Century: The beginning of studies exploring the complex interplay between the gut and distant immune organs, including the spleen. John Bienenstock, a Canadian immunologist, developed the concept of the "common mucosal immune system" which proposed that mucosal immune sites, including the gut, were interconnected with other distant sites.
- Early 2000s: Advances in sequencing technologies accelerated microbiome research, leading to a rapid increase in the understanding of gut microbiota's influence on the immune system, and scientists such as Jeffery Gordon, and Lita Proctor contributed by making this area of research more accessible to the scientific community.
- 21st Century: The rise of the concept of the gut-spleen axis as a field of research, focusing on the complex communication between the gut and spleen, and its role in health and disease. Researchers such as Laurence Zitvogel (Gustave Roussy Institute) explored the role of the gut microbiome in modulating anti-cancer immune responses, with findings showing the gut microbiome's effect on the spleen and its role in systemic immunity.
- 2010s onwards: A growing appreciation of the interconnected nature of the immune system has led to more research on the mechanisms of communication between the gut and spleen, including the roles of specific immune cells, cytokines, and microbial metabolites.
- Ongoing Research (2024 and beyond): Current research explores therapeutic approaches targeting the gut-spleen axis to manage chronic inflammatory conditions, autoimmune diseases, and cancer, including the use of fecal microbiota transplantation (FMT), prebiotics, probiotics, and dietary interventions. Research focuses on optimizing these treatments to achieve more consistent and predictable results.
Introduction
Have you ever paused to consider the hidden communication pathways within your body, particularly how your gut might be influencing a seemingly distant organ like your spleen? It’s easy to view our organs as isolated entities, but the reality is that they're part of an intricate, interconnected system. Today, we’re going to explore the fascinating relationship between your gut and your spleen, and delve into how this connection plays a pivotal role in your immune surveillance, while also encouraging critical thinking about different approaches to health.
We’ve been exposed to a lot of information about immune responses and interventions. This article isn’t about promoting any particular viewpoint; instead, it’s about exploring the science and mechanisms behind the gut-spleen axis, as well as the potential of interventions like fecal microbiota transplantation (FMT). We'll also highlight strategies for supporting your body's natural defenses. The aim here is to empower you with knowledge so that you can make your own informed choices. It's essential to always approach health information with a critical eye, as explored in our article on critical thinking. Let’s dive in and uncover the secrets of this often-overlooked connection!
Section 1: The Spleen: More Than Just a Filter ️
Let's start by looking at the spleen, an organ that plays a central role in your immune system. You might think of it mainly as a blood filter, but it’s much more than that.
1.1 What Does the Spleen Do?
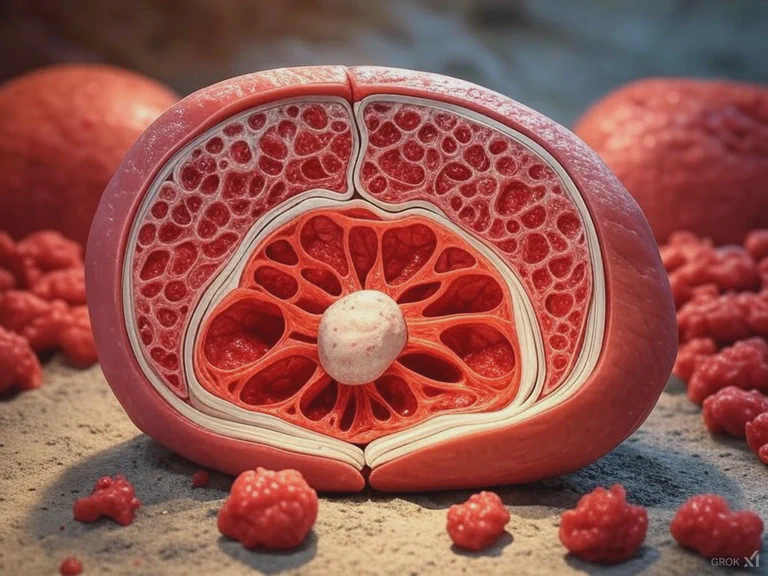
The spleen is a soft, fist-sized organ located in the upper left abdomen. It acts as a major filter for your blood, removing old or damaged red blood cells, and also various pathogens and debris. However, its roles extend far beyond this. The spleen is also a crucial player in immune surveillance, constantly monitoring your blood for pathogens, abnormal cells, and other harmful substances. It’s like the body’s internal security checkpoint, but also a place where the immune system can develop.
1.2 Key Immune Functions of the Spleen
The spleen is involved in a variety of immune processes:
- Filtering Blood: The spleen filters blood, removing pathogens (like bacteria and viruses), damaged cells, and other debris, which can then be disposed of, playing a vital role in preventing systemic infections.
- Immune Cell Activation: The spleen contains a specialized compartment called the white pulp, where immune cells, like lymphocytes (T cells and B cells), are activated, and can initiate a coordinated immune response.
- Antibody Production: The spleen is a crucial site for the production of antibodies, which are essential for fighting off infections. B cells in the spleen mature into plasma cells, producing a large number of antibodies, a key component of humoral immunity.
- Immune Surveillance: It constantly monitors the blood, identifying and responding to anything that shouldn't be there, like pathogens and abnormal cells, thus maintaining continuous immune protection.
- Red blood cell recycling: The spleen not only filters blood but also breaks down old and damaged red blood cells, which is crucial for maintaining blood health.
1.3 Why Understanding the Spleen Matters
Understanding the spleen's functions is crucial, as it sheds light on the body’s complex immune system. Any disruption in spleen function can impact your ability to fight off infections, clear damaged cells, and maintain overall health, potentially leading to a variety of immune-related disorders. It also provides a critical link to our next area: the connection with the gut.
Learn more about the fundamentals of the immune system and the important role of the liver in gut health.
Section 2: The Gut Microbiome: A World Within
Now, let's turn our attention to the gut microbiome, the trillions of bacteria, viruses, fungi, and other microorganisms that reside in your digestive tract.
2.1 What is the Gut Microbiome?
The gut microbiome is a complex and dynamic ecosystem. It's not just a collection of random organisms; it's a highly interactive community that plays a key role in your health, affecting your metabolism, immune system, and even brain function. It helps to break down food that our bodies can’t digest on its own, synthesize vitamins, and crucially, shapes your immune system by interacting with immune cells in the gut lining.
2.2 The Microbiome's Influence on Immunity
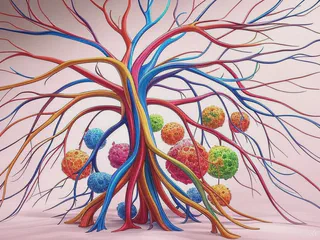
The gut microbiome is increasingly recognized for its pivotal role in shaping immune responses:
- Immune Cell Development: The gut microbiome helps to train and develop immune cells, such as lymphocytes (including T cells and B cells), which are crucial for fighting infections and maintaining immune homeostasis. Early colonization of the gut by beneficial bacteria is crucial for the proper development of the immune system.
- Gut Barrier Function: A healthy gut microbiome maintains the integrity of the gut barrier, which is a lining of epithelial cells. This prevents harmful substances, such as pathogens and bacterial toxins, from entering the bloodstream and potentially affecting other organs, contributing to systemic inflammation.
- Inflammation Regulation: The gut microbiome influences inflammation, a key process in immune responses, and can both promote and resolve inflammation, maintaining the balance required for a healthy immune response. Dysbiosis can lead to chronic low-grade inflammation throughout the body.
- Immune Response Modulation: By interacting with immune cells, the gut microbiome influences how our body reacts to pathogens, and may influence the body's response to various health challenges, including responses to vaccines and other medical interventions. It contributes to the development of immune tolerance, preventing overreaction to harmless substances.
2.3 What Happens When the Microbiome is Imbalanced?
An imbalance in your gut microbiome, known as dysbiosis, can have various consequences. This can involve a reduction in beneficial bacteria, and an increase in less helpful ones, causing a disruption of the gut environment. This can lead to:
- Increased Inflammation: Dysbiosis can cause systemic inflammation by allowing bacterial products to enter the bloodstream. This can impact various organs, including the spleen.
- Impaired Immune Function: It can also compromise the immune response by disrupting the proper training and activation of immune cells. This may lead to increased susceptibility to infections.
- Disrupted Gut Barrier: Dysbiosis may also contribute to leaky gut (increased intestinal permeability), allowing substances from the gut to enter the bloodstream, triggering inflammation and immune responses.
Understanding the complex interplay between your gut microbiome and your immune system is crucial for maintaining optimal health and resilience, as well as enabling a critical approach to health information. Discover more about the importance of the gut-immune connection.
Section 3: The Gut-Spleen Axis: A Communication Network
Now, let’s delve into the fascinating connection between your gut and your spleen, known as the gut-spleen axis. This is not a direct physical connection, but rather a complex communication network involving various pathways.
3.1 How Does the Gut Communicate with the Spleen?
This communication occurs through several different channels:
- Immune Cells: Immune cells, such as dendritic cells, macrophages, and lymphocytes, which are present in both the gut and the spleen, can travel between the two, and carry signals through the lymphatic system.
- Circulating Molecules: Various molecules, including inflammatory molecules (like cytokines), microbial products (such as lipopolysaccharide (LPS)), and short-chain fatty acids (SCFAs), can travel through the bloodstream to the spleen, influencing the spleen’s immune activity.
- The Lymphatic System: The lymphatic system is a network of vessels that transports immune cells and other molecules, linking the gut and the spleen, serving as a conduit for the trafficking of immune cells and signaling molecules between the two sites.
- Nervous System: The gut and brain are connected through the enteric nervous system and the vagus nerve, which could have some influence on communication pathways to the spleen via neuro-immune pathways, which are still not fully understood.
3.2 The Spleen’s Response to Gut Signals
The spleen reacts to signals coming from the gut in a variety of ways:
- Modulation of Immune Cells: Signals from the gut microbiome can influence the activation and function of immune cells in the spleen, including lymphocytes (T cells and B cells), affecting their ability to respond to pathogens.
- Response to Pathogens: If the gut microbiome detects a pathogen, signals may be sent to the spleen, leading to a targeted immune response, which involves the activation of immune cells to eliminate pathogens effectively.
- Filtering of Microbial Products: The spleen can filter and remove any substances coming from the gut, including microbial products such as bacterial fragments and toxins, preventing them from causing systemic harm, playing an important role in immune surveillance.
3.3 The Importance of This Connection
This two-way communication between the gut and the spleen is essential for maintaining a balanced immune system. When the communication pathways are disrupted, it can have negative consequences for overall health, contributing to inflammatory and immune disorders. The gut-spleen axis is important for promoting immune surveillance and ensuring an adequate and appropriate response to pathogens, as well as the resolution of inflammation. The health of the gut is also closely linked to the health of your blood vessels, as explored in our article on the gut-vascular connection.
Explore the importance of prebiotics and probiotics for your gut microbiome, and understand the crucial role of the gut microbiome for your overall health
Section 4: The Gut-Spleen Axis and Immune Responses
Now, let’s look at how this connection between your gut and your spleen can influence your body’s immune responses, particularly in the context of information about interventions for health.
4.1 The Gut-Spleen Axis in Immune Surveillance
The gut-spleen axis plays an essential role in maintaining immune surveillance, ensuring that your body is constantly monitoring and responding to potential threats. This may involve the following:
- Detection of Pathogens: The gut microbiome sends signals to the spleen when it detects pathogens in the gut, triggering an immune response, involving the activation of immune cells to fight the pathogen.
- Antigen Presentation: The spleen also acts as a site where antigens (foreign substances) are presented to immune cells. This process is critical for triggering a targeted immune response and establishing immunological memory.
- Memory Responses: The gut-spleen axis is also important for establishing immunological memory. Once the body has encountered a pathogen, it will remember it, and the next time the response will be faster and more efficient due to the presence of memory cells in both the spleen and the gut.
4.2 The Impact of Dysbiosis on Spleen Function
Disruptions to the gut microbiome can have far-reaching effects on the spleen and its ability to carry out its immune surveillance functions:
- Inflammatory Signals: Dysbiosis can lead to inflammatory signals being sent to the spleen, potentially disrupting its normal function and leading to chronic low-grade inflammation.
- Impaired Immune Response: It can also compromise the spleen’s ability to effectively identify and respond to pathogens, leading to an increased susceptibility to infections and autoimmune disorders.
- Altered Immune Cell Function: Dysbiosis may cause immune cells in the spleen to respond less effectively, hindering the body's ability to fight off infections and clear damaged cells, which can also lead to more inflammation.
4.3 Supporting the Gut-Spleen Axis: Insights from Research
Research, such as that published in mSphere, has explored how interventions aimed at modulating the gut microbiota may influence spleen function. Specifically, the study found that fecal microbiota transplantation (FMT), using gut microbiota that had been improved with alginate oligosaccharide (AOS), could help to rescue spleen function after it had been disrupted by an anti-cancer drug. This research suggests the importance of gut health in supporting immune function and highlights a potential area of interest for exploring gut-based therapies. It's important to approach this and all health information with a critical mindset. More research is needed to fully understand the potential and limitations of FMT and other gut-based therapies in supporting spleen function and overall immune health.
Explore the relationship between the gut and the lungs, and how the anti-inflammatory diet can help to manage your health, and how your gut impacts the immune system.
Section 5: Supporting Your Gut-Spleen Axis Naturally
Let's explore some strategies for supporting your gut-spleen axis, and acknowledge the value of a balanced approach to health.
5.1 Dietary Strategies
- Emphasize Fiber-Rich Foods: Consume plenty of fruits, vegetables, legumes, and whole grains to nourish your gut microbiome by promoting the growth of beneficial bacteria. Be mindful of how you cook your food, and learn more about gut-friendly cooking methods.
- Include Polyphenol-Rich Options: Add berries, green tea, and dark chocolate for their antioxidant and anti-inflammatory properties, which help to reduce inflammation and promote a healthy gut environment. Check out the benefits of EGCG in green tea.
- Limit Processed Foods and Sugar: Minimize processed foods and added sugars, which can disrupt your gut microbiome by promoting the growth of harmful bacteria, and be aware of the impact of processed foods and artificial sweeteners .
5.2 Targeted Nutritional Approaches
- Probiotics: Consider probiotic supplements to support a balanced gut microbiome by increasing the number of beneficial bacteria, and explore the benefits of probiotics for your gut.
- Prebiotics: Include prebiotic-rich foods to feed the beneficial bacteria, which will help them to thrive and produce beneficial compounds, and read more about prebiotics for supporting a healthy microbiome.
- Omega-3 Fatty Acids: Incorporate foods rich in omega-3s to help regulate inflammation and promote a balanced immune response. Discover the value of omega-3 fatty acids in your diet.
- Vitamin D: Ensure sufficient vitamin D for supporting your immune function, as it helps to modulate immune responses, and understand the importance of vitamin d for your overall health.
5.3 Lifestyle Choices
- Regular Exercise: Get your body moving, as exercise can help to modulate the gut microbiome and support circulation, reducing inflammation and supporting overall health, and check out the benefits of exercise for your gut.
- Stress Management: Manage chronic stress to reduce its negative impact on your gut and overall health, as stress can disrupt the gut microbiome and immune function, while learning more on the gut and stress connection.
- Adequate Sleep: Prioritize sleep to support your immune system and overall health, as sleep is crucial for immune cell function and the regulation of inflammation. Explore the link between sleep and immunity.
5.4 Personalization
Remember, everyone's needs are unique, and it's important to approach health choices with awareness and a critical perspective. Factors like genetics, lifestyle, and pre-existing conditions will influence your individual needs. Creating a gut-friendly kitchen is a great start to a more personalized approach to health.
Section 6: Considering Individual Factors and Future Research
6.1 Individual Variability
It’s vital to remember that individual responses vary greatly. Factors contributing to this variability include:
- Genetic Predisposition: Genetic variations can influence the function of the immune system, the composition of the gut microbiome, and therefore, the communication along the gut-spleen axis. You can learn more on the topic of gut health and genetic expression.
- Pre-existing Conditions: Existing health conditions such as autoimmune diseases, chronic infections, and inflammatory disorders can impact the gut-spleen axis and immune responses, making individuals respond differently to the same interventions. You may also want to explore the relationship between gut health and autoimmune conditions.
- Lifestyle Choices: Lifestyle factors such as diet, stress, sleep patterns, and exercise can significantly influence the gut microbiome and immune function, highlighting the importance of a holistic approach to health. You can discover the impact of gut health in the modern world.
6.2 Future Research
- Long-Term Studies: More research is needed to fully understand the long-term interactions between the gut and spleen in diverse populations, as well as the impact of different interventions over time, to inform long-term strategies for health.
- Personalized Approaches: Focus on personalized strategies is crucial, taking into account genetic and lifestyle factors, as well as pre-existing conditions. This approach can enable more effective interventions for the gut-spleen axis.
- Targeted Interventions: Research into specific approaches that can positively impact the gut-spleen axis is necessary, including identifying which strategies or combinations of strategies are most effective for different individuals and conditions. You can also explore the concept of gut microbiome and personalized medicine.
Conclusion: Supporting Natural Resilience
The gut-spleen axis is a remarkable example of the interconnectedness within our bodies. By understanding this relationship and making conscious choices to support a balanced gut microbiome, you can enhance your body's natural immune surveillance and promote overall health. It’s important to approach health decisions with a critical and informed perspective, allowing you to make the best choices for your unique needs, and to be aware of the complex relationships within the body.
Disclaimer: The information provided in this article is intended for general knowledge and informational purposes only, and does not constitute medical advice. It is essential to consult with a qualified healthcare professional for any health concerns or before making any decisions related to your treatment plan, medications, or supplements. Self-treating can be risky, and it's vital to collaborate with someone who can create a plan specifically tailored to your individual needs.
Further Reading:
- Gut: The Inside Story of Our Body's Most Underrated Organ by Giulia Enders
- The Mind-Gut Connection: How the Hidden Conversation Within Our Bodies Impacts Our Mood, Our Choices, and Our Overall Health by Emeran Mayer
- Fiber Fueled: The Plant-Based Gut Health Program for Losing Weight, Restoring Your Health, and Optimizing Your Microbiome by Will Bulsiewicz
- Brain Maker: The Power of Gut Microbes to Heal and Protect Your Brain--for Life by David Perlmutter
- The Clever Guts Diet: How to Revolutionize Your Body from the Inside Out by Michael Mosley