Timeline of Key Discoveries
- Early 1900s: Initial observations of the gut microbiome's role in digestion, with scientists like Élie Metchnikoff (Nobel laureate) proposing the "theory of autointoxication" and highlighting the potential benefits of lactic acid bacteria in the gut, sparking early interest in the gut's role in health.
- 1910-1960s: A period of relative dormancy in microbiome research, with focus shifting towards antibiotic development and germ theory, leading to a temporary overshadowing of the beneficial roles of gut bacteria.
- 1970s: The gut's significance as an immune organ began to emerge, revealing its critical role beyond just digestion. Researchers like Robert Good, considered the "father of modern immunology," demonstrated the importance of the gut-associated lymphoid tissue (GALT) in immune development and the gut's role in immune tolerance. ️
- 1980s: Researchers uncovered the first connections between gut bacteria and inflammation, hinting at a more complex relationship than previously thought. Jeffery Gordon (University of Washington) started pioneering studies using gnotobiotic (germ-free) mice, allowing for controlled experiments that began to unravel the complex interplay between gut bacteria and host physiology.
- 1990s: The discovery of short-chain fatty acids (SCFAs) and their profound importance in gut and overall health opened up a new area of study. Scientists such as Gary Gibson (University of Reading) and Glenn Reid (Western University) began to characterize SCFAs and their impact on the gut lining and systemic health, leading to new dietary and therapeutic strategies.
- Early 2000s: The growing evidence of gut dysbiosis (an imbalance in gut bacteria) impacting systemic health made it clear that gut health has far-reaching implications. Alessio Fasano (Harvard Medical School) made significant contributions by identifying zonulin as a key regulator of intestinal permeability, and highlighting how gut barrier dysfunction could contribute to various conditions.
- 2010s: The concept of the gut-brain axis gained prominence, along with connections to other organ systems, recognizing the extensive communication networks of the body. John Cryan and Ted Dinan (University College Cork) popularized research demonstrating how the gut microbiome communicates with the brain, influencing mood, behavior, and even neurodegenerative diseases.
- 2015 onwards: The emergence of the "gut-vascular axis" as a distinct field of research began, uncovering links to cardiovascular health, metabolic disorders, and immune responses, solidifying the importance of vascular health. Scientists such as Filip Swirski (Massachusetts General Hospital) conducted groundbreaking work connecting inflammation, gut dysbiosis, and the development of atherosclerosis, highlighting the systemic impact of gut health on vascular integrity. 🩸
- 2020: The outbreak of the COVID-19 pandemic shifted global research priorities, with an intense focus on understanding the SARS-CoV-2 virus and developing effective vaccines. Initial studies began to explore the relationship between gut health and COVID-19 severity, with evidence suggesting that individuals with dysbiotic gut microbiomes experienced worse outcomes.
- 2020-2021: The rapid development and rollout of mRNA vaccines led to observations of rare but significant adverse events, notably cases of myocarditis (inflammation of the heart muscle), particularly in younger males, leading to intense investigation.
- 2021 Onwards: Scientists such as Peter McCullough, Aseem Malhotra, and Charles Hoffe were among the early voices raising concerns about potential cardiovascular risks associated with mRNA vaccines, drawing attention to case studies and early data. Sabine Hazan began to investigate the role of the gut microbiome in the vaccine response, and also the effects of spike proteins on the gut microbiome, and the correlation to vaccine adverse events. These researchers contributed by highlighting potential links between the spike protein, inflammation, and vascular dysfunction. Many cardiologists contributed with their observations in clinical practice.
- Research began to explore the role of the spike protein, produced by the body following vaccination, in potentially triggering inflammatory and thrombotic (blood clot) events. Investigations into the mechanisms behind mRNA vaccine-associated myocarditis pointed towards immune system activation, inflammatory responses, and potential endothelial dysfunction.
- Studies also focused on understanding individual susceptibility to adverse events, with a growing appreciation for the role of genetic factors, pre-existing conditions, and lifestyle habits in modulating immune responses and vaccine-associated risks.
- 2024 and Beyond: Continued investigation into the long-term effects of mRNA interventions on the gut-vascular axis, the mechanisms behind rare adverse events, and strategies to optimize immune responses. There is a push for further understanding of the gut microbiome's role in vaccine effectiveness and safety, including exploring personalized approaches to enhance immune resilience, and reduce the incidence of adverse events. The focus also turned to potential treatments and remedies, while also promoting critical thinking and individual informed decision-making. Current research continues to investigate the complexities of how mRNA vaccines interact with the gut-vascular axis, with an emphasis on personalized medicine approaches. A major focus is on developing strategies to improve immune responses, reduce adverse effects, and to develop personalized approaches to vaccine administration, tailoring the response to individual characteristics such as gut health, genetic makeup, and lifestyle. Critical thinking, as outlined in our article on critical thinking, plays a vital role in navigating these complex issues, promoting informed decision-making, and enabling people to make responsible choices based on the latest scientific information.
Introduction
Have you ever wondered how your gut, the place where food is digested, might affect the health of your blood vessels? It's easy to think of our body parts as working separately, but they're actually deeply connected. Today, we're diving into one of the most fascinating of these connections: the gut-vascular axis. This connection is particularly relevant as we navigate various health challenges and ongoing discussions around pharmaceutical interventions and immune responses.
We’ve all been exposed to a lot of information recently, particularly around the 2020 pandemic and a certain type of vaccine. This has led to a lot of FUD (fear, uncertainty, and doubt) for some people, and mistrust in medical professionals. But beyond the headlines, there's a complex story unfolding about how our inner ecosystem, our gut microbiome (the collection of bacteria, viruses, fungi, and other microbes in our digestive tract) influences our immune system and our blood vessels. We're not here to rehash a particular narrative; rather, we're going to look at the science, explore the mechanisms, and give you practical, evidence-based strategies for improving your health through your gut. It's important to be able to make your own informed decisions, and to think critically, as we discuss in our article on critical thinking. So, let's explore this intricate relationship and how it impacts your health.
Section 1: The Unsung Architect: Hyaluronan and Its Two Faces ♂️
Let's begin with a molecule you may not have heard of, but plays a huge role in your body: hyaluronan (HA). It's a behind-the-scenes player, but it's absolutely essential.
1.1 What Exactly is Hyaluronan?
Think of HA like a long sugar chain, similar to a string of beads, that's found all over your body. You can find it in your skin, joints, and blood vessels. Interestingly, it comes in two main forms: High Molecular Weight HA (HMW-HA) and Low Molecular Weight HA (LMW-HA). They have very different roles, like two sides of a coin. One, HMW-HA, is generally stable and helpful, while the other, LMW-HA, can sometimes cause problems.
1.2 HMW-HA: A Structural Component
HMW-HA, the larger version, helps keep your tissues hydrated, kind of like a sponge holding water. It also acts as a structural support in the extracellular matrix (the space between cells), and it has anti-inflammatory properties to help keep your body balanced. HMW-HA is also important for keeping your blood vessels healthy.
1.3 LMW-HA: A Potential Inflammatory Trigger
Now here’s where it gets interesting. When HMW-HA breaks down into smaller pieces, it becomes LMW-HA. This breakdown can occur through a few ways:
- Enzymatic Cleavage (The Scissors): Special enzymes called hyaluronidases (HYAL1 and HYAL2) act like tiny scissors, cutting the large HA chains into smaller pieces.
- Oxidative Stress (The Wrecking Ball): Unstable molecules, known as Reactive Oxygen Species (ROS), which increase during inflammation, can act like wrecking balls, breaking down the HA chains.
- Mechanical Stress (The Battering Ram): The simple act of blood flowing through your vessels can put stress on HA, causing it to break over time.
The size of HA is crucial. When it gets broken down below a certain point (around 200 kDa, a measurement of size), it can lose its helpful properties and contribute to inflammation.
1.4 Why This Matters: The HA Connection
Understanding how HA works can help us understand some of the complex responses our bodies have. It highlights the delicate balance within us and how things can be influenced.
You can learn more about how important hydration is for healthy tissues and the role of antioxidants in protecting the body. It's also worth looking into the innate and adaptive immune system and how inflammation plays a part in health conditions.
Section 2: The Endothelial Barrier: Your Blood Vessels and Their Integrity
Let’s now focus on the endothelial barrier, which is the lining of your blood vessels. This layer is really important for maintaining healthy blood vessels.
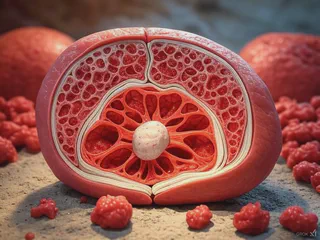
2.1 What Exactly is the Endothelial Barrier?
These ECs are held together by special junctions. Tight junctions act like seals, and adherens junctions, especially a protein called VE-cadherin, provide structural integrity and control how the cells stick together.
2.2 When the Endothelial Barrier is Compromised
When these junctions are not working correctly, the integrity of the blood vessel lining can be disrupted. This can occur due to:
- Inflammatory Mediators: Certain molecules can make the ECs contract, creating gaps in the barrier.
- Oxidative Stress: Unstable molecules (ROS) can damage nitric oxide (NO), a key molecule for blood vessel health, and weaken the barrier.
- HA Fragmentation: LMW-HA may also disrupt the protective layer on the ECs, making the barrier more fragile.
2.3 Potential Consequences of Barrier Dysfunction
When the endothelial barrier is compromised, it can lead to:
- Edema (Swelling): Increased permeability can cause fluids to leak into the surrounding tissues, leading to swelling.
- Thrombosis (Blood Clots): Damage to the barrier can expose collagen, activating the clotting process and increasing the risk of blood clots.
- Atherosclerosis (Plaque): Increased permeability may allow substances to enter the arterial walls, contributing to the build-up of plaque.
You can find information on how to manage stress to reduce inflammation, how omega-3 fatty acids can affect vascular health, and the connection between the gut and heart health.
Section 3: The Gut-Vascular Axis: A Complex Relationship ↔️
Now, let’s consider the gut-vascular axis, the complex relationship between the gut and blood vessels, where each influences the other.
3.1 What is the Gut-Vascular Axis?
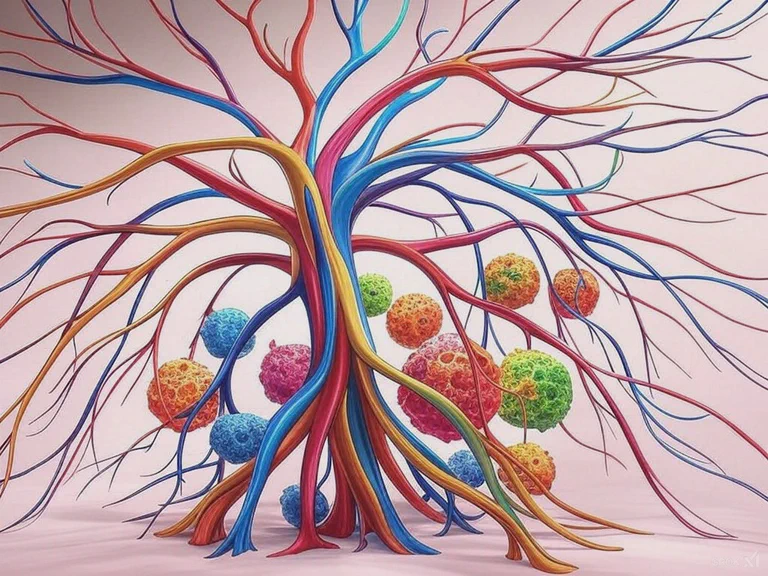
Think of the gut-vascular axis as a communication network that links your gut microbiome with your blood vessels. It's a complex interaction of immune responses, inflammatory signals, and metabolic processes.
3.2 How the Gut Microbiome Influences Blood Vessels
Your gut microbiome is becoming more and more recognized for its major role in overall health, and can have effects on the vascular system:
- Short-Chain Fatty Acids (SCFAs): When you eat fiber, gut bacteria produce SCFAs like butyrate. These molecules have been studied for their potential to maintain the gut barrier and influence inflammation.
- Inflammatory Signals: Dysbiosis (an imbalance in your gut) can cause inflammatory substances to leak into the bloodstream, which can affect blood vessels.
- Immune System Modulation: Your gut microbiome is closely linked to your immune system. Imbalances can lead to an overactive immune response affecting both your gut and your blood vessels.
3.3 The Gut-Vascular Axis and Immune Responses
How your body responds to vaccines can also be affected by the gut-vascular axis:
- Modulating Inflammation: The state of your gut microbiome can affect the inflammatory response after a vaccine.
- Protecting the Endothelial Barrier: A balanced microbiome can help keep the endothelial barrier healthy.
- Influencing Immune Response: Gut bacteria may influence how effective the immune response is.
3.4 The Effects of Disruption
Imbalances in this axis may lead to:
- Increased Inflammation: Dysbiosis can contribute to inflammation, impacting blood vessels.
- Altered Immune Response: An imbalanced gut microbiome can lead to an altered immune response.
- Changes in Vascular Health: Dysbiosis can also contribute to negative changes in vascular health.
You can learn more about the gut-immune connection and the potential benefits of probiotics and prebiotics, as well as how an anti-inflammatory diet could improve your health.
Section 4: Considering mRNA Interventions and the Gut-Vascular Axis
Let's now look at how mRNA interventions and their components might interact with the gut-vascular axis.
4.1 How mRNA Interventions Work
These interventions deliver mRNA to cells, which then produce a specific protein. The idea is that this triggers an immune response, which trains the body to recognize the virus.
4.2 Potential (Indirect) Effects on the Gut-Vascular Axis
The body’s responses to these interventions may lead to some changes:
- Inflammatory Mediators: Activation of the immune system might result in the release of inflammatory molecules, which could impact blood vessels.
- HA Fragmentation: The inflammatory response could also increase the activity of enzymes that break down HA.
- Vascular Permeability: Inflammatory mediators may change how permeable blood vessels are, potentially making them more prone to leakage.
- GAG Shedding: GAGs (Glycosaminoglycans) are complex sugar molecules that form a slippery, protective layer on the surface of the endothelial cells lining blood vessels. This layer helps to maintain smooth blood flow and prevent blood cells and other components from sticking to the vessel walls. Think of it like the Teflon coating on a pan, preventing things from sticking, or the lining of a pipe, ensuring a smooth and unimpeded flow. GAG shedding refers to the loss of this protective layer from the surface of endothelial cells. This process can be triggered by inflammatory conditions, oxidative stress, and the action of certain enzymes, including hyaluronidases. When GAGs are shed, the inner lining of the blood vessels becomes more exposed and vulnerable, which may increase the risk of vascular problems, including thrombosis. Furthermore, this GAG shedding can be linked to an increase in thrombosis, as without the slippery coating of GAGs, blood cells and platelets may adhere more easily to the damaged endothelial surface, promoting clot formation. Studies suggest that the spike protein itself may be able to cause GAG shedding, directly damaging endothelial cells, and contributing to vascular issues. Additionally, the spike protein can interact directly with endothelial cells via receptors like ACE2, which can trigger signaling pathways that promote inflammation, and endothelial dysfunction.
4.3 The Gut Microbiome's Role
The gut microbiome can also play a role in these responses:
- A Balanced Microbiome: A balanced gut might help to regulate inflammation.
- An Imbalanced Microbiome: An imbalanced gut may make any inflammatory effects worse.
4.4 What Current Information Suggests
It’s important to know that people can have different responses, and there is ongoing research into these interactions. It’s important to empower yourself with knowledge, and approach the topic with critical thinking.
You can learn more about the gut-lung axis, how you can manage inflammation with diet, and how your gut impacts the immune system.
Section 5: Strategies for Supporting Natural Resilience
Let's discuss some strategies that focus on supporting natural resilience, while acknowledging that individuals make their own informed choices about health interventions.
5.1 Dietary Considerations
- Fiber-Rich Foods: Eat plenty of fruits, vegetables, legumes, and whole grains to support your gut microbiome. It's also useful to explore gut-friendly cooking methods.
- Polyphenol-Rich Foods: Berries, green tea, and dark chocolate are great sources of antioxidants and anti-inflammatory compounds. You can also look into the power of EGCG in Green Tea.
- Limit Processed Foods & Sugar: Consider limiting processed foods and sugars, which can disrupt the microbiome and promote inflammation. Explore the impact of processed foods and the effect of artificial sweeteners.
5.2 Targeted Nutritional Support
- Probiotics: Consider a high-quality probiotic to support a balanced microbiome, and learn about the potential benefits of probiotics.
- Prebiotics: Support your probiotics with prebiotic-rich foods, and consider the benefits of prebiotics.
- Omega-3s: Incorporate foods rich in omega-3 fatty acids to support healthy inflammation levels. You can learn more about omega-3 fatty acids.
- Vitamin D: Ensure you have sufficient levels of Vitamin D, which is vital for immune function. You can also research the importance of Vitamin D.
5.3 Lifestyle Factors
- Regular Exercise: Incorporate regular exercise, which may benefit your gut microbiome and blood flow. Explore the benefits of exercise for your gut.
- Stress Management: Practice relaxation techniques to reduce the negative impact of stress on your gut and overall health. You can also consider the link between the gut and stress.
- Adequate Sleep: Quality sleep is essential for immune function and overall health. Explore the link between sleep and immunity.
5.4 A Personalized Approach
Remember that everyone is unique, so a personalized approach can be helpful. Consider creating a gut-friendly kitchen for a holistic approach.
Section 6: Individual Factors and Future Research
6.1 Individual Variability
It's essential to recognize that people may have different responses to health challenges. Several factors contribute to this:
- Genetic Predisposition: Our genes can influence how our bodies respond to different stimuli. You can learn more about gut health and genetic expression.
- Pre-existing Conditions: Conditions like diabetes, autoimmune diseases, and cardiovascular issues can affect immune responses. Consider the impact of gut health and autoimmune conditions.
- Lifestyle: Daily habits, including diet, stress levels, and sleep patterns, can affect your overall health. You can also look into the impact of the gut on the modern world.
6.2 Looking Forward: The Future of Research
- Long-Term Studies: We need more research to understand the long-term effects of different interventions on the gut-vascular axis.
- Personalized Approaches: A focus on individual factors is needed to understand the subtleties of individual responses. Learn more on the topic of gut microbiome and personalized medicine.
- Gut Microbiome Modulation: More research is needed on the impact of specific interventions on vaccine responses.
Conclusion: Supporting Your Body's Natural Resilience
The gut-vascular axis is a complex and important system in our bodies, playing a crucial role in our immune response and overall health. While the specific effects of interventions on the gut and blood vessels are still being researched, it’s clear that supporting a healthy gut microbiome is essential. By focusing on evidence-based strategies, you can take a proactive role in supporting your health. It is important to use critical thinking, and to empower yourself with knowledge.
Disclaimer: The information in this article is for general knowledge and informational purposes only, and doesn't constitute medical advice. It’s essential to talk with a healthcare professional for any health concerns, or before making decisions about your treatment plan, medications, or supplements. Self-treating can be risky, and it’s important to work with someone who can create a plan specifically for your needs.
Further Reading:
- Gut: The Inside Story of Our Body's Most Underrated Organ by Giulia Enders
- The Mind-Gut Connection: How the Hidden Conversation Within Our Bodies Impacts Our Mood, Our Choices, and Our Overall Health by Emeran Mayer
- Fiber Fueled: The Plant-Based Gut Health Program for Losing Weight, Restoring Your Health, and Optimizing Your Microbiome by Will Bulsiewicz
- Brain Maker: The Power of Gut Microbes to Heal and Protect Your Brain--for Life by David Perlmutter
- The Clever Guts Diet: How to Revolutionize Your Body from the Inside Out by Michael Mosley