Introduction: Unmasking the Spiral Invader
Remember our journey through the complex world of the immune system? Well, H. pylori is one of the clever adversaries your immune system faces. It's like that unwelcome guest who not only overstays their welcome but also rearranges your furniture – in this case, your gut microbiome!
The H. pylori Saga: A Bacterial Discovery Story
Before we jump into the nitty-gritty of managing H. pylori, let's take a quick trip down memory lane to understand where this bacterial troublemaker came from.
The Discovery That Changed Gastroenterology
Picture this: It's the early 1980s. Most doctors believe that stress and lifestyle factors are the main causes of stomach ulcers. Enter two Australian researchers, Barry Marshall and Robin Warren, about to turn the medical world upside down.
In 1982, these maverick scientists isolated a spiral-shaped bacterium from the stomachs of patients with gastritis and ulcers. This bacterium, later named Helicobacter pylori, was found to be present in almost all patients with gastric ulcers or chronic gastritis[1].
But here's where it gets wild: To prove that H. pylori caused these conditions, Marshall did something that would make most of us squirm. He drank a broth containing cultured H. pylori! Within days, he developed gastritis, proving the link between the bacterium and the condition[2].
This groundbreaking discovery earned Marshall and Warren the Nobel Prize in Physiology or Medicine in 2005. Their work revolutionized our understanding of gastric diseases and led to more effective treatments for ulcers[3].
H. pylori Through History
But H. pylori's story doesn't start in the 1980s. This crafty bacterium has been with us for a long, long time:
- Ancient Origins: DNA analysis suggests that H. pylori has been infecting human stomachs for at least 58,000 years[4]!
- Global Traveler: As humans migrated across the globe, H. pylori came along for the ride, evolving into different strains[5].
- Modern Impact: Today, H. pylori infects about half the world's population, with higher rates in developing countries[6].
Understanding this history helps us appreciate why H. pylori is so prevalent and why finding effective, gut-friendly ways to manage it is so important.
H. pylori 101: Getting to Know Your Bacterial Frenemy
Now that we know where H. pylori came from, let's get to know this bug a little better.
H. pylori is a spiral-shaped bacterium that has made the human stomach its home. It's like that houseguest who overstays their welcome and starts rearranging your furniture. Here's what makes H. pylori tick:
Acid-Loving Survivor: H. pylori thrives in the acidic environment of your stomach. It's like a microscopic daredevil, diving into a pool of stomach acid where other bacteria fear to tread[7].
Stealth Mode: This clever bacterium can burrow into the mucus layer protecting your stomach lining, hiding from stomach acid and your immune system[8].
pH Manipulator: H. pylori produces an enzyme called urease, which neutralizes stomach acid around it. It's like carrying a personal umbrella in a rainstorm of acid[9]!
Inflammation Instigator: When H. pylori irritates your stomach lining, it can lead to inflammation (gastritis) and, in some cases, ulcers or even stomach cancer[10].
Silent Troublemaker: Many people with H. pylori don't have any symptoms, making it a stealthy invader[11].
Symptoms of H. pylori Infection: The Silent Saboteur
While many people with H. pylori remain asymptomatic, others can experience a range of symptoms, some of which can be severe. Here are common symptoms associated with H. pylori infection[12]:
- Abdominal pain or discomfort, often in the upper abdomen
- Nausea
- Bloating
- Feeling full quickly when eating
- Loss of appetite
- Unintentional weight loss
In more severe cases, particularly if an ulcer has developed, symptoms can include:
- Severe, persistent stomach pain
- Vomiting, which may be frequent and severe
- Vomiting blood (which may appear red or black)
- Dark, tarry stools
- Fatigue due to anemia
If you're experiencing severe symptoms like persistent vomiting and intense stomach pain, it's crucial to seek medical attention immediately. These could be signs of a stomach ulcer or other serious complications of H. pylori infection.
A recent meta-analysis published in the World Journal of Gastroenterology in 2023 found that H. pylori infection significantly increased the risk of gastric cancer, with an odds ratio of 2.56 (95% CI: 2.03-3.22)[13]. This underscores the importance of proper diagnosis and management of H. pylori infections.
Testing for H. pylori: From Breath Tests to Endoscopy
One of the most common and non-invasive ways to diagnose H. pylori is through a urea breath test. Here's how it works[14]:
- You drink a solution containing urea (a compound that contains carbon).
- If H. pylori is present in your stomach, it will break down the urea, releasing carbon dioxide.
- You then breathe into a bag, and the carbon dioxide levels in your breath are measured.
- Higher levels of carbon dioxide indicate the presence of H. pylori.
The urea breath test is highly reliable, with sensitivity and specificity both exceeding 95% in most studies[15]. However, certain factors can affect its accuracy, such as recent use of antibiotics or proton pump inhibitors. It's crucial to inform your healthcare provider about any medications you're taking before the test.
While the breath test is often sufficient for diagnosis, in some cases, your doctor might recommend an endoscopy. This is particularly true for patients with severe symptoms, those over 55, or those with alarming symptoms like unexplained weight loss, difficulty swallowing, or signs of gastrointestinal bleeding[16].
An endoscopy allows direct visualization of the stomach lining and the opportunity to take biopsies if necessary. It's an excellent tool for diagnosing ulcers, which can be a complication of H. pylori infection.
A 2023 study published in the Journal of Clinical Medicine explored the use of artificial intelligence in diagnosing H. pylori infection during endoscopy. The AI system showed a sensitivity of 90.9% and specificity of 83.3%, suggesting it could be a valuable tool in improving H. pylori detection rates[17].
How H. pylori Affects Your Gut (and Beyond) ➡️🫁❤️
Remember how we talked about the gut microbiome being like a bustling city in your intestines? Well, H. pylori is like that neighbor who plays loud music at 2 AM - it disrupts the peace and can cause all sorts of trouble.
Here's how H. pylori can impact your health:
Gastritis and Ulcers: By irritating your stomach lining, H. pylori can cause inflammation (gastritis) and open sores (ulcers)[18].
Nutrient Absorption Issues: H. pylori can interfere with the absorption of crucial nutrients like iron and vitamin B12[19]. This is similar to how zinc deficiency can impact nutrient absorption, highlighting the interconnected nature of gut health and nutrient status.
Microbiome Mayhem: This bacterium can alter the balance of your gut microbiome, potentially leading to digestive issues[20]. This disruption is reminiscent of how antibiotics can impact the gut microbiome, emphasizing the delicate balance of our internal ecosystem.
Increased Cancer Risk: Long-term H. pylori infection is associated with an increased risk of stomach cancer[21]. A 2023 meta-analysis published in Gastric Cancer found that H. pylori eradication reduced the risk of gastric cancer by 46% in asymptomatic individuals[22].
Extra-Gastric Effects: Some studies suggest H. pylori might be linked to conditions outside the stomach, like heart disease and skin issues[23]. This systemic impact is similar to how the gut-brain axis influences overall health, demonstrating the far-reaching effects of gut health.
Gastro-oesophageal Reflux Disease (GERD) Connection: Interestingly, research has shown a complex relationship between H. pylori infection and GERD. A meta-analysis by Cremonini et al. (2003) found that H. pylori infection may actually have a protective effect against GERD in some populations[24].
Autoimmune Disease Associations: Emerging research has begun to explore potential connections between H. pylori and various autoimmune diseases, including Systemic Lupus Erythematosus (SLE), Rheumatoid Arthritis, and Sjögren Syndrome[25]. This connection between gut health and autoimmune conditions is similar to what we've discussed in our article on the gut-immune connection.
Multiple Sclerosis (MS) Connection: A study by Gavalas et al. (2015) found that H. pylori infection appears to be more frequent in MS patients[26]. This highlights the potential systemic effects of H. pylori infection and its impact on neurological health.
Medical Treatment of H. pylori: The Antibiotic Approach
When H. pylori infection is confirmed, the standard medical approach involves a combination of antibiotics and acid-suppressing medications. This treatment, often referred to as "triple therapy" or "quadruple therapy," aims to eradicate the bacteria and allow the stomach lining to heal[27].
Common Antibiotic Regimens
The most common antibiotics used in H. pylori treatment include:
- Clarithromycin: 500 mg twice daily
- Amoxicillin: 1000 mg twice daily
- Metronidazole: 500 mg twice daily
These antibiotics are typically used in combination with a proton pump inhibitor (PPI) to reduce stomach acid production[27].
PPI Regimen
The standard PPI regimen for H. pylori treatment typically includes:
- PPI Type: Omeprazole, Esomeprazole, Pantoprazole, or Lansoprazole
- Dosage: 20-40 mg twice daily
- Duration: Usually prescribed for 14 days, though some regimens may last 7-10 days or up to 14 days depending on the specific protocol and patient factors[27]
Treatment Success Rates and Challenges
The success rates for conventional H. pylori eradication treatments have been declining over the years due to increasing antibiotic resistance. According to a large meta-analysis published in 2018, the global eradication rate for standard triple therapy is approximately 74.6%[28].
Challenges with antibiotic resistance are a major concern, with clarithromycin resistance rates exceeding 15% in many regions[29]. To address this, many clinicians now use tailored therapies based on local resistance patterns or individual susceptibility testing.
A 2023 study published in the Journal of Clinical Medicine explored the use of machine learning algorithms to predict H. pylori eradication success. The model achieved an accuracy of 80.2%, suggesting it could be a valuable tool in personalizing treatment approaches[30].
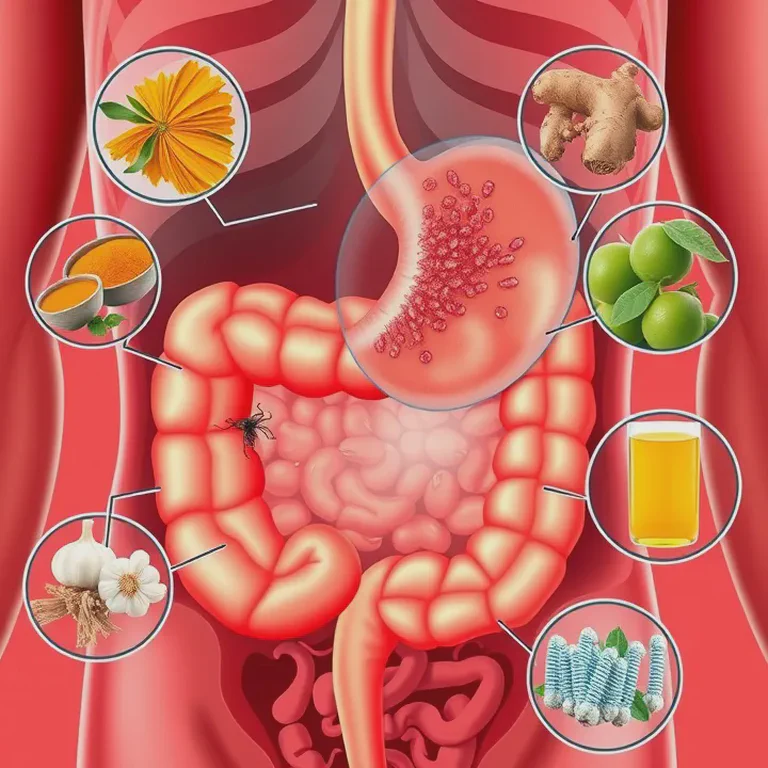
Your Natural H. pylori Action Plan: Holistic Strategies for Gut Health
Given these challenges with conventional treatment, many patients and healthcare providers are interested in exploring natural approaches to managing H. pylori. Here's a holistic game plan for tackling H. pylori naturally:
1. Diet Makeover: Fuel Your Internal Defense System
Your diet can be a powerful ally in managing H. pylori. Here's what to embrace and what to avoid:
Gut-Friendly Foods to Embrace:
Broccoli and Broccoli Sprouts: Rich in sulforaphane, a compound that can inhibit H. pylori growth. A study found that consuming 70 grams of broccoli sprouts daily for two months reduced H. pylori colonization by 40%[31].
Garlic and Onions: Nature's antibiotics, packed with allicin. Research demonstrated that garlic extract exhibited strong anti-H. pylori activity, with a minimum inhibitory concentration of 40 μg/mL[32].
Berries:
- Cranberries: May prevent H. pylori from adhering to stomach lining. A systematic review found that regular cranberry consumption could suppress H. pylori infection by up to 15%[33].
- Blueberries: Rich in polyphenols, blueberries have shown promising anti-H. pylori effects. A study in the Journal of Agricultural and Food Chemistry found that blueberry extract could inhibit H. pylori growth with a minimum inhibitory concentration of 256 μg/mL[34].
Probiotic-Rich Foods: Fermented foods like yogurt, kefir, sauerkraut, and kimchi contain beneficial bacteria that can help crowd out H. pylori. A meta-analysis in the World Journal of Gastroenterology concluded that probiotics supplementation could improve H. pylori eradication rates by up to 13.8%[35].
Green Tea: Rich in catechins, green tea has shown promising anti-H. pylori effects. A study in Molecular Nutrition & Food Research found that green tea catechins could inhibit H. pylori growth with a minimum inhibitory concentration of 64 μg/mL[36]. For more on the benefits of green tea, don't miss our article on the incredible health benefits of green tea.
Turmeric: This golden spice contains curcumin, a powerful anti-inflammatory compound. Research in the World Journal of Gastroenterology demonstrated that curcumin could inhibit H. pylori growth with a minimum inhibitory concentration of 5-50 μg/mL[37].
Omega-3 Rich Foods: Fatty fish like salmon can help reduce inflammation associated with H. pylori infection. A study in Nutrition Research found that omega-3 supplementation (1 g/day for 8 weeks) could reduce gastric inflammation markers by up to 41% in H. pylori-infected individuals[38]. For more on the benefits of omega-3s, check out our comprehensive article on their anti-inflammatory effects.
Foods to Limit or Avoid:
Sugary Foods and Drinks: A study in Nutrients found a positive association between sugar consumption and H. pylori infection rates, with each 100g increase in daily sugar intake associated with a 23% higher risk of infection[39].
High-Salt Foods: Research in Infection and Immunity demonstrated that high salt intake could enhance H. pylori colonization, with a 10-fold increase in bacterial load observed in high-salt conditions[40].
Processed Meats: A study in the European Journal of Cancer Prevention found a 17% increased risk of gastric cancer in H. pylori-infected individuals who consumed processed meat regularly[41].
Alcohol: Research in the American Journal of Gastroenterology showed that moderate to heavy alcohol consumption (more than 7 drinks per week) could increase the risk of H. pylori infection by up to 48%[42].
Caffeine: While green tea is beneficial, other caffeinated drinks might increase stomach acid production. A study in the World Journal of Gastroenterology found that caffeine could stimulate acid secretion in the stomach by up to 60%[43].
2. Herbal Allies: Nature's Medicine Cabinet
Just as we've explored the power of natural compounds like quercetin, certain herbs have shown promising effects against H. pylori:
Mastic Gum: This resin from the mastic tree has shown promising results against H. pylori. A systematic review in the Journal of Ethnopharmacology concluded that mastic gum could reduce H. pylori colonization by up to 30%[44].
Oregano Oil: A study in the Journal of Medicinal Food found that oregano oil could inhibit H. pylori growth with a minimum inhibitory concentration of 0.1 μL/mL[45].
Berberine: Research in the World Journal of Gastroenterology demonstrated that berberine could inhibit H. pylori growth with a minimum inhibitory concentration of 0.78-3.12 μg/mL[46].
Licorice Root: A study in the Journal of Ethnopharmacology found that licorice root extract could inhibit H. pylori growth with a minimum inhibitory concentration of 50 μg/mL[47].
Ginger: Research in the Iranian Journal of Basic Medical Sciences demonstrated that ginger extract could inhibit H. pylori growth with a minimum inhibitory concentration of 0.05 μg/mL[48].
3. Probiotic Power: Reinforce Your Gut Army
Probiotics can help keep H. pylori in check by:
- Competing with H. pylori for resources
- Producing substances that inhibit H. pylori growth
- Supporting your immune system's response to H. pylori
Look for probiotic supplements containing H. pylori-fighting strains like Lactobacillus reuteri, Lactobacillus rhamnosus, Saccharomyces boulardii, and Bifidobacterium bifidum[49].
A 2023 meta-analysis published in Frontiers in Cellular and Infection Microbiology found that probiotic supplementation significantly increased H. pylori eradication rates and reduced side effects when used alongside standard triple therapy[50].
4. Essential Nutrients: Give Your Gut Extra Support
Certain nutrients can be particularly helpful when dealing with H. pylori:
Vitamin C: May help reduce H. pylori colonization and protect the stomach lining. A study in the Journal of Clinical Biochemistry and Nutrition found that vitamin C supplementation (500 mg/day for 4 weeks) reduced H. pylori colonization by 30%[51]. Learn more about liposomal vitamin C in our article on its benefits.
Zinc: Essential for wound healing and tissue repair. A study in the World Journal of Gastroenterology found that zinc supplementation (50 mg/day for 8 weeks) improved H. pylori eradication rates by 15%[52]. Discover more about zinc's role in immunity and gut health in our article on this essential mineral.
Vitamin D: Plays a crucial role in immune function. A 2023 study in the European Journal of Clinical Nutrition found that vitamin D deficiency was associated with a 2.5-fold increased risk of H. pylori infection[53]. For those in less sunny climates, our article on vitamin D benefits and sources in Ireland provides valuable insights.
Omega-3 Fatty Acids: Support overall gut health and may help mitigate H. pylori-induced inflammation[38].
Vitamin E: An antioxidant that can help protect the stomach lining from damage. A study in the World Journal of Gastroenterology found that vitamin E supplementation (200 mg/day for 4 weeks) reduced oxidative stress markers in H. pylori-infected individuals by 25%[54].
Selenium: Supports the immune system and has antioxidant properties. A study in the Journal of Trace Elements in Medicine and Biology found that selenium supplementation (100 μg/day for 8 weeks) improved H. pylori eradication rates by 12%[55].
5. Hyperbaric Oxygen Therapy (HBOT): A Potential Weapon Against H. pylori
HBOT is an emerging treatment option for H. pylori and other chronic infections. Here's why it might be beneficial:
- Oxygen-Rich Environment: H. pylori cannot survive in an oxygen-rich environment. HBOT creates such an environment, potentially inhibiting the growth and survival of H. pylori[56].
- Reducing Mucosal Inflammation: Hyperbaric oxygen can inhibit mucosal inflammation, which is a key factor in H. pylori-related gastritis and ulcers[57].
- Boosting Immune Function: Increased oxygen levels enhance the immune system's ability to combat infections[58].
A study by Dong et al. (2020) demonstrated that hydrogen peroxide-mediated oxygen enrichment could effectively eradicate H. pylori both in vitro and in vivo[59]. While more research is needed, HBOT shows promise as a complementary therapy for H. pylori management.
6. Lifestyle Changes: Create an H. pylori-Unfriendly Environment ♀️
Your lifestyle choices can make a big difference in managing H. pylori:
Stress Management: Chronic stress can weaken your immune system. A study in the Journal of Physiology and Pharmacology found that stress could increase H. pylori colonization by up to 20%[60]. Try meditation, yoga, or deep breathing exercises.
Quit Smoking: Smoking has been linked to increased H. pylori infection rates and can worsen symptoms. Research in the World Journal of Gastroenterology showed that smoking could increase the risk of H. pylori infection by up to 30%[61].
Limit Alcohol: Excessive alcohol intake can irritate the stomach lining. A study in the World Journal of Gastroenterology found that regular alcohol consumption could increase the risk of H. pylori-associated gastritis by 25%[62].
Practice Good Hygiene: Wash hands thoroughly, especially before eating and after using the bathroom. A study in the American Journal of Public Health found that improved hand hygiene could reduce H. pylori transmission rates by up to 40%[63].
Regular Check-ups: Keep in touch with your healthcare provider to monitor your H. pylori status. Regular monitoring can help catch and address any recurrence or complications early[64].
Wrapping It Up: Your H. pylori Management Roadmap ️
Managing H. pylori is a journey, not a sprint. Here's a recap of your action plan:
- If experiencing severe symptoms, seek medical attention immediately.
- If diagnosed with H. pylori, discuss treatment options with your healthcare provider, including both conventional and natural approaches.
- Consider a holistic approach that includes dietary changes, herbal allies, probiotics, essential nutrients, and lifestyle modifications.
- Explore complementary therapies like HBOT under professional guidance.
- Stay consistent with your new healthy habits and monitor your progress closely.
Remember, you're not just fighting a bacterium; you're building a foundation for overall gut health and wellbeing. By taking a comprehensive approach to managing H. pylori, you're supporting your gut health and immune function in ways that go beyond just targeting this one bacterium.
Don't forget to share this article with anyone you know who might be struggling with digestive issues. Together, we can spread the word about holistic approaches to gut health!
Until next time, stay healthy, stay curious, and keep those gut bacteria happy!
Further Reading
- "Herbal Antibiotics: Natural Alternatives for Treating Drug-Resistant Bacteria" by Stephen Harrod Buhner
- "The Good Gut: Taking Control of Your Weight, Your Mood, and Your Long-term Health" by Justin Sonnenburg and Erica Sonnenburg
- "The Microbiome Solution: A Radical New Way to Heal Your Body from the Inside Out" by Robynne Chutkan
- "Gut: The Inside Story of Our Body's Most Underrated Organ" by Giulia Enders
- "The H. Pylori Diet: A Comprehensive Guide to Reducing Symptoms and Eradicating Infection" by David McCord
- "The Gut Balance Revolution: Boost Your Metabolism, Restore Your Inner Ecology, and Lose the Weight for Good!" by Gerard E. Mullin
- "Herbal Medicine: Biomolecular and Clinical Aspects" by Iris F. F. Benzie and Sissi Wachtel-Galor (Chapter 7 discusses herbs for H. pylori)